- 翰林提供學(xué)術(shù)活動(dòng)、國(guó)際課程、科研項(xiàng)目一站式留學(xué)背景提升服務(wù)!
- 400 888 0080
IB DP Biology: SL復(fù)習(xí)筆記6.4.1 Ventilation: Function & Structures
Ventilation
- Ventilation?can be defined as
- The replacement of older air in the lungs with fresh air from the body's external environment
- Ventilation is essential for the effective?exchange of gases?in the lungs
- The?exchange?of oxygen and carbon dioxide occurs between the?alveoli?and the capillaries in the lungs
- Gases are exchanged by?simple?diffusion?which requires a?concentration gradient
- This gradient is maintained by
- Ventilation
- The?continuous flow of blood?in the capillaries
The impact of ventilation
- Ventilation maintains?concentration gradients?of oxygen and carbon dioxide between air in the alveoli and blood flowing in adjacent capillaries
- Breathing in?fresh air from the surrounding environment increases the concentration of oxygen in the air inside the alveoli
- Breathing out?removes carbon dioxide
- This means that after ventilation, compared to the blood found in adjacent capillaries, the alveoli have
- Higher oxygen levels
- Lower carbon dioxide levels
- This ensures that oxygen continues to?diffuse?from the alveoli into the capillaries, while carbon dioxide continues to diffuse from the capillaries into the alveoli
- Both gases move down their?concentration gradient
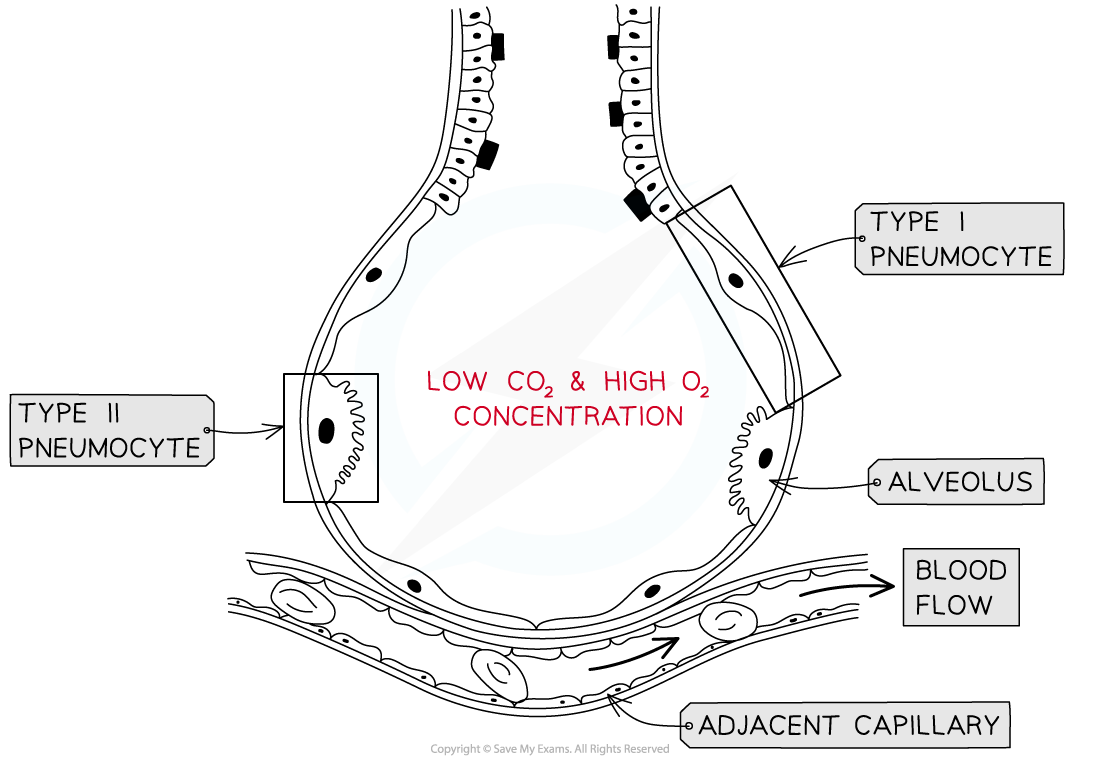
Ventilation maintains a concentration gradient between the air in the alveolus and the blood in the adjacent capillary
Type I Pneumocytes
- The alveoli are specifically adapted for gas exchange as they collectively have a?very large surface area?and the alveolar walls are only one cell thick which provides a?short diffusion distance
- The alveolar walls are also known as the alveolar epithelium
- Type I pneumocytes?are extremely?thin alveolar cells?which make up the majority of the alveolar epithelium
- They are adapted to maximise the rate of gas exchange by providing a?short diffusion distance
- The capillary walls are also only?one cell thick?which means there is usually less than?0.5μm?between the air in the alveoli and the blood, this?maximises the rate of diffusion
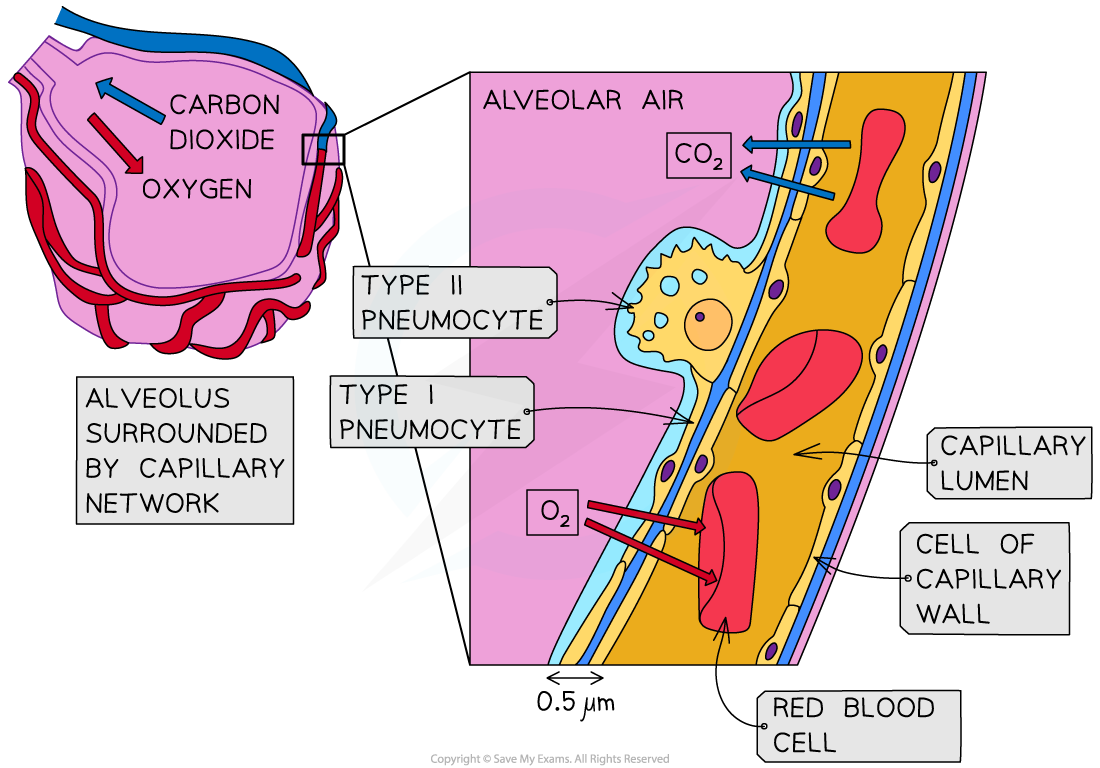
The thin type I pneumocyte cells and the thin capillary walls provide a short diffusion distance to maximise gas exchange
Type II Pneumocytes
- Type II pneumocytes are?rounded cells?which secrete a solution that coats?the epithelium of the alveoli
- They occupy a much smaller proportion of the alveolar epithelium than the type I pneumocytes; around 5%
- The solution released by type II pneumocytes contains?pulmonary surfactant
- Pulmonary surfactant has?hydrophobic?tails and?hydrophilic?heads
- The molecules form a monolayer with the hydrophobic tails facing the alveolar air
- Pulmonary surfactant?reduces?surface tension, maintaining alveolar?shape?and?preventing the?sacs sticking?together
- This prevents the alveoli, and therefore the lungs, from?collapsing
- The solution also aids gas exchange
- The layer of moisture provided by the solution allows?oxygen to dissolve?before it diffuses into the blood
- Carbon dioxide?diffuses from the moist surface before it is removed in exhalation
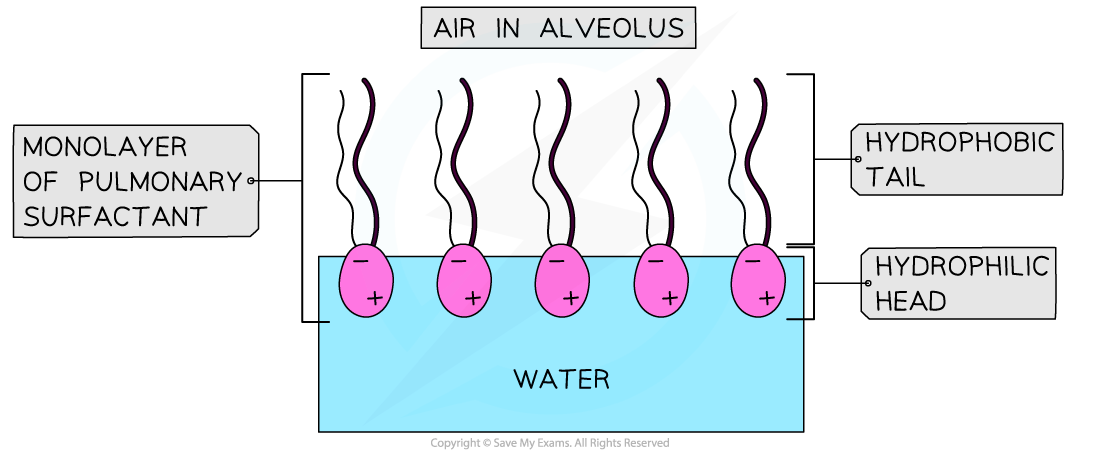
The type II pneumocyte cells in the alveoli produce a solution containing pulmonary surfactant which reduces surface tension
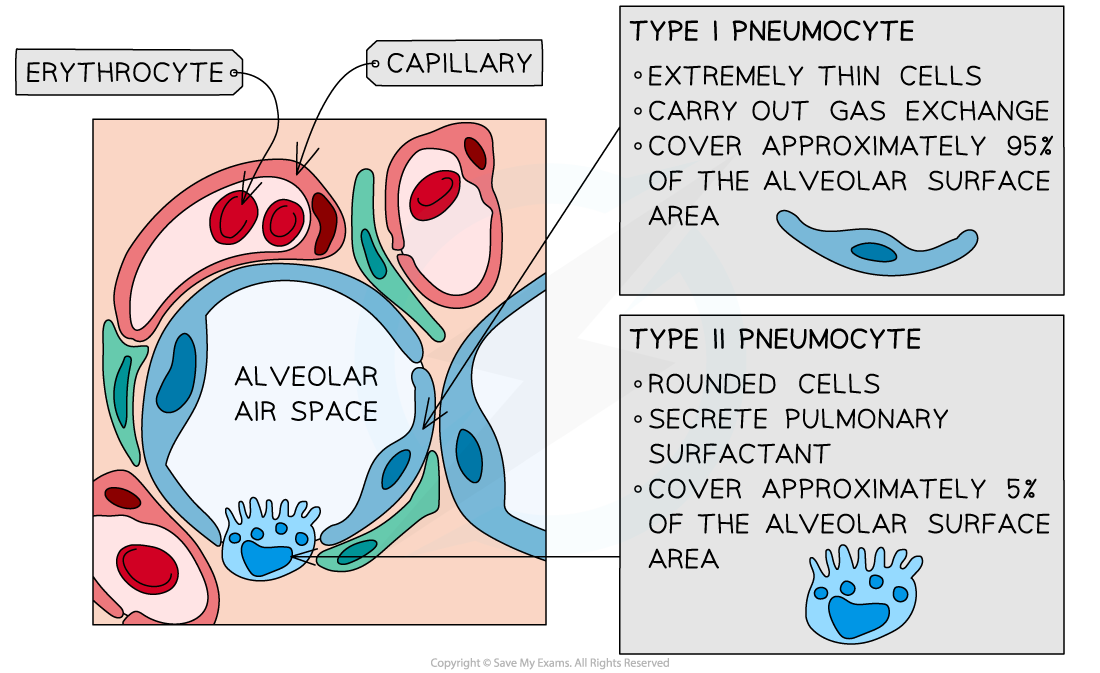
The alveolar epithelium is made up of type I and type II pneumocyte cells
Air Pathway
- Air moves in through the nose and mouth before it is carried to the lungs through the?trachea
- The?trachea?is a tube supported by?rings of cartilage?which help to support its shape and ensure it stays open, while allowing it to move and flex with the body
- The?trachea?divides to form the two?bronchi?(singular bronchus) with walls also strengthened with cartilage and has a layer of smooth muscle?which can?contract?or?relax?to change the diameter of the airways.
- One bronchus leads to each lung
- Bronchioles?branch off the two bronchi to form a network of narrow tubes
- The walls of the bronchioles are lined with a layer of?smooth muscle?to alter the diameter of the bronchiole tubes
- This helps to regulate the flow of air into the lungs by dilating when more air is needed and constricting when e.g. an allergen is present
- Groups of?alveoli?are found at the end of the bronchioles
- Each alveolus is surrounded by an extensive network of?capillaries?to provide a?good blood supply?for maximum gas exchange
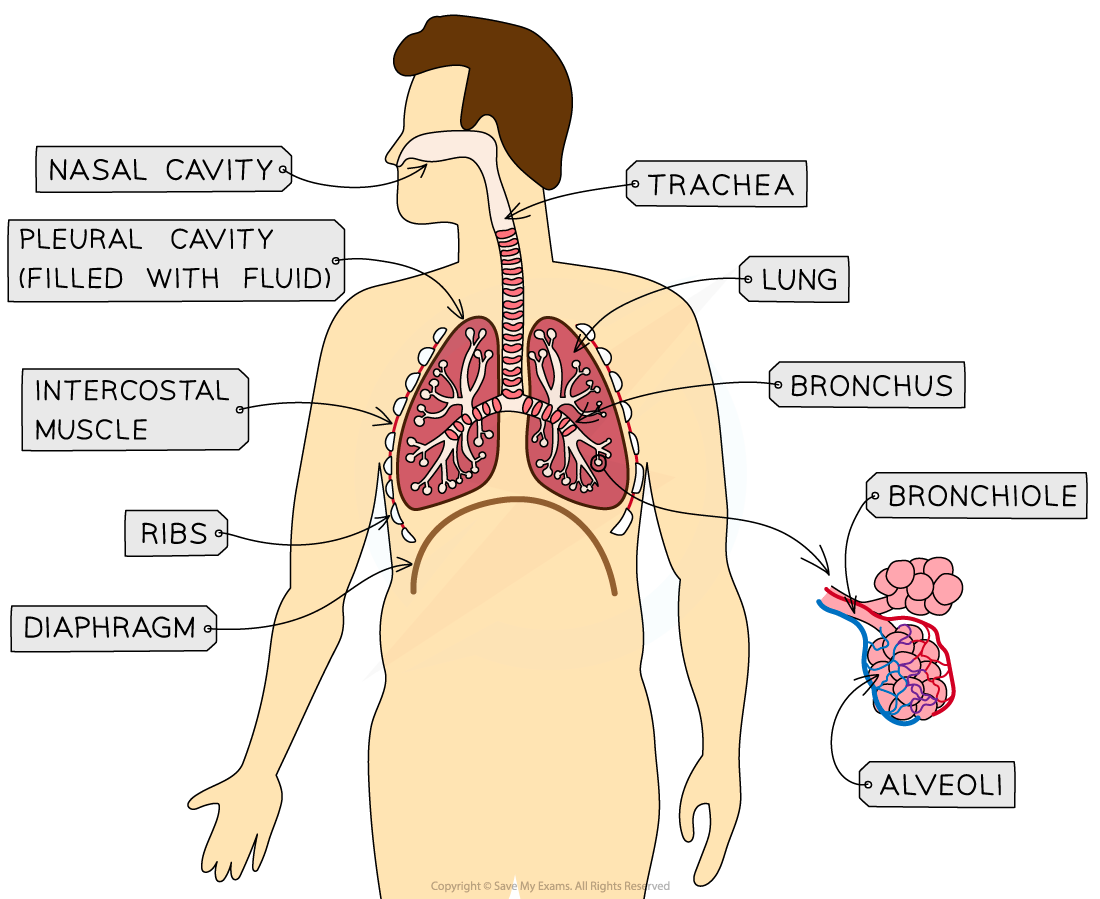
The main structures of the human gas exchange system
轉(zhuǎn)載自savemyexams

最新發(fā)布
? 2025. All Rights Reserved. 滬ICP備2023009024號(hào)-1